This article found it’s way to my inbox, so I decided to look further into the details: AI Can Predict Prognosis After Lumbar Disc Herniation. The claim made is “Machine learning models can inform patients and clinicians about prognosis after lumbar disc herniation surgery…” [1]
Lumbar disc herniation surgery is common, but not always effective for everyone. The current prediction models have had limited accuracy due to small datasets available. This study developed and validated machine learning models using a large national spine registry (NORspine) to predict individual patient outcomes in disability and paint improvement after surgery. Outcomes included measured patient improvements using ODI and NRS from baseline to 12 months. All potential preoperative predictors available in the NORspine registry were used. 25 predictor variables were included, covering patient demographic characteristics, comorbidity, clinical characteristics, analgesics use, and type of operation.
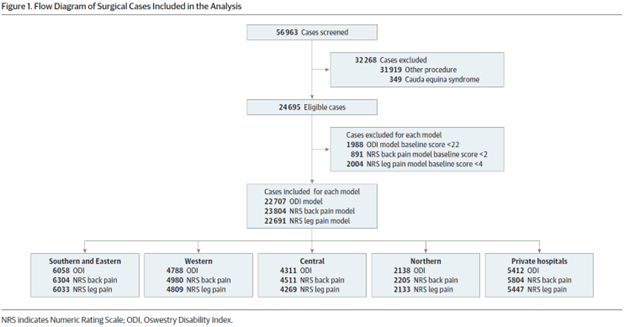
To ensure the adequacy of the data set and how many predictors could be included, a statistical calculation was used to estimate sample size needed for this study, which estimated that 2551 patients would be required for the model development, corresponding to 766 events and an even per parameter of 15.3. In the end, 22,707 surgical cases (21,161 patients) who underwent operations for lumbar disc herniation were eligible for inclusion in the primary analysis. (I want to make a note in this area that the balance of males to females was 12,952 to 9,755 respectively. However, because the adequate calculated sample set was 2,551 patients, both numbers provide sufficient data points to draw a reasonable conclusion with data analysis.)
The predictive performance of the 7 different machine learning algorithms was compared using estimates of the random effects meta-analysis per algorithm and outcome. The models performed well across different regions and hospitals, with good discrimination (ability to distinguish success and failure) and calibration (accuracy of predictions). No significant advantage of machine learning over logistic regression in this case. The key findings for model performance were:
- C statistic (discrimination) > 0.81 for disability and > 0.74 for pain.
- Models performed well in real-world settings (different regions and hospitals).
- Comparable or better than previous prediction models.
It should be noted that limitations of the study included:
- Missing Data: Some important features and outcome data were missing, limiting the model’s potential accuracy.
- Data Suboptimality: Some data types in the registry (e.g., medication, healthcare use) were limited in detail, potentially impacting prediction.
- Outcome Definition: The cutoff for “treatment success” used may not be universally agreed upon.
- Sample Bias: The study only looked at surgical patients, excluding potential outcomes of non-surgical treatment.
- Optimal Timing: The study didn’t address the optimal timing for lumbar discectomy surgery.
It was found that these models offer several key advantages:
- High accuracy: They effectively distinguish between successful and unsuccessful outcomes (high discrimination).
- Real-world application: They rely on data readily available before surgery, making them practical for implementation.
- Scalability: Their compatibility with electronic medical records allows for easy integration and individual patient risk assessment.
By informing both patients and surgeons about potential outcomes, these models can assist in personalized decision-making and potentially improve surgical success rates.
Future Work:
- Explore including missing data in model development and updating it with new features.
- Enrich the model with data from electronic health records for better prediction.
- Consider alternative outcome definitions for validation in other settings.
- Investigate the potential outcomes of non-surgical treatment for high-risk patients.
- Study the optimal timing of surgery for improving outcomes.
References:
[1] Elana Gotkine, Meeta Shah, M.D., Elana Gotkine, & Meeta Shah, M.D. (2024, February 9). AI can predict prognosis after lumbar disc herniation surgery. Healthday-en. https://www.healthday.com/healthpro-news/bone-and-joint/ai-can-predict-prognosis-after-lumbar-disc-herniation-surgery
Journal Article:
Berg B, Gorosito MA, Fjeld O, et al. Machine Learning Models for Predicting Disability and Pain Following Lumbar Disc Herniation Surgery. JAMA Netw Open. 2024;7(2):e2355024. doi:10.1001/jamanetworkopen.2023.55024
Photo by ThisIsEngineering: https://www.pexels.com/photo/code-projected-over-woman-3861969/

Leave a comment